Healthcare providers around the world are increasingly phasing out paper-based patient records in favor of digital systems. This shift is especially notable in low-resource settings - from rural clinics in sub-Saharan Africa and remote parts of South America to island hospitals in the Caribbean and underserved areas of the United States. The reasons are clear: paper records are inefficient, error-prone, and vulnerable, while electronic health records (EHRs) offer speed, accuracy, and resilience. International health organizations have emphasized that digital health solutions like EHRs are essential for improving care in low- and middle-income countries. Ministries of Health, clinic administrators, and NGOs are recognizing that adopting digital health records is not just a tech upgrade, but a vital step toward better patient outcomes and more efficient healthcare operations.
The Hidden Costs and Risks of Paper-Based Records
Relying on paper files may seem straightforward, but it carries heavy hidden costs and risks for clinics:
- Frequent loss and misfiling: It's estimated that 15% of all paper documents are misplaced and 7.5% are lost entirely. In healthcare, a lost or misfiled patient chart can lead to treatment delays or medical errors. For example, an archival survey in a rural South African community found that only 39% of requested patient records could be located, meaning the majority were missing. Such gaps in records can be dangerous for patient care and undermine trust in the system.
- Wasted time and productivity: Paper systems force staff to spend enormous time on paperwork. The typical office worker loses about four weeks per year searching for misfiled, mislabeled, or lost documents. Healthcare personnel in particular spend twice as much time on paperwork as those in other industries , shuffling through folders instead of caring for patients. One report noted that every misfiled document can cost an organization $125 in lost productivity. In a busy clinic, these inefficiencies add up to longer wait times and shorter attention for each patient.
- Poor accessibility and coordination: Paper charts are burdensome to share and access, often requiring physically transporting files or making phone calls to find information. This lack of quick access can slow down decision-making and even jeopardize patient outcomes. Doctors and nurses must dig through cabinets to retrieve past records, and if a patient is referred to another facility, their history might not follow. Patients frequently end up repeating tests or procedures because prior results on paper weren't available - studies have found that patients undergo duplicate procedures, or miss needed ones, when records are incomplete
- Security and privacy risks: Unlike modern EHR systems that use encryption and access controls, anyone can open an unlocked file cabinet. Paper records can be read, copied, or even stolen without leaving a trace. This raises serious privacy concerns, especially with sensitive health information. There's also no easy backup - if a paper file is lost or destroyed, the information is gone forever.
- Vulnerability to disasters: Paper records are literally made of paper - they can burn, rot, or wash away. A flood, fire, or hurricane can obliterate years of medical history overnight. When Hurricane Katrina struck New Orleans in 2005, tens of thousands of patients lost their entire medical histories as paper files disintegrated or washed out to sea. In that disaster, only about a quarter of doctors had electronic records, and the rest saw decades of handwritten charts wiped out. The lesson has been stark: clinics that remain on paper are one disaster away from losing critical patient data.
Simply put, paper-based recordkeeping is "inefficient" and error-prone in ways modern healthcare can no longer afford. It hampers the quality of care, burdens the staff, and exposes patients to avoidable risks. These inefficiencies are driving decision-makers in low-resource settings to seek a better way.
Benefits of Digital Health Records in Resource-Limited Settings
Moving to electronic health records offers transformative benefits, even (and especially) for clinics with limited resources. Here are some key advantages data has shown:
- Faster access and better decision-making: Digital records put patient information at providers' fingertips. Instead of hunting for a paper folder, a clinician can retrieve a complete medical history with a few clicks, even remotely. This instantaneous access speeds up treatment decisions. For instance, EHR implementations in Ghana's emergency departments improved the accuracy and timeliness of patient information, helping doctors make quicker, better decisions in critical moments. In general, studies confirm that electronic systems are faster and more accurate, reducing redundant paperwork and allowing staff to focus on patient care.
- Reduced errors and improved safety: A well-implemented EHR can dramatically cut down on medical errors. In various settings, switching from paper to electronic records has been associated with a 20-30% reduction in documentation errors and a significant boost (15-25%) in the accuracy of patient data. By flagging drug interactions or allergies and ensuring legible, complete documentation, EHRs help prevent the mistakes that happen with illegible handwriting or forgotten notes. In the U.S. and other high-income countries, widespread EHR adoption led to a 54% drop in medication errors. The same safety improvements are now being observed in low-resource environments as they digitize. For example, in Rwanda, introducing an EHR system for chronic disease management increased data completeness by 20% and reduced patients' average blood sugar (HbA1c) levels significantly, indicating better-managed care. Such outcomes show that digital records directly contribute to safer, higher-quality treatment.
- Better care coordination and continuity: Digital health records enable seamless information sharing among departments and even across different facilities. This is a game-changer in regions where patients might visit multiple clinics or see traveling specialists. With paper files, important details often fall through the cracks. But with EHRs, all providers can access the same up-to-date information. In Trinidad and Tobago, for instance, the health system's digital transformation includes integrated health information systems that link patient records across hospitals and clinics, so a patient's history is available wherever they go. Similarly, many Caribbean hospitals (e.g. in Barbados) now use networked electronic medical records, ensuring that even if a person goes to a different facility or a rural health outpost, their data is readily accessible. This continuity of care means fewer repeated tests, smoother referrals, and ultimately better outcomes for patients.
- Enhanced efficiency and cost savings: While there is an upfront cost to implementing EHRs, over time digital systems can save money for clinics and health programs. They reduce the administrative burden - automating tasks like chart pulls, report generation, and billing. Studies have noted that EHR systems tend to boost revenue and lower operational costs by streamlining workflows. For resource-strapped clinics, even small efficiency gains (like seeing a few extra patients per day because less time is spent on paperwork) make a big difference. Moreover, electronic records open the door to telemedicine and remote consultations, which can expand a clinic's reach without major new infrastructure. During the COVID-19 pandemic, many places leveraged digital records plus telehealth to maintain services. For example, Jamaica's use of the ECHO tele-education model and telemedicine tools was facilitated by digital platforms, helping rural doctors get specialist input and training virtually. All these efficiency gains contribute to a more sustainable and scalable healthcare system.
- Data for public health and planning: Digital records create structured data that can be aggregated and analyzed for important insights. Health ministries and NGOs can monitor disease trends, track vaccination coverage, or identify gaps in care much more easily with electronic data than by collecting stacks of paper forms. In fact, a core goal of "going digital" is to support evidence-based decision-making. As one report noted, meaningful use of EHRs allows clinicians to compile data on patient populations and pinpoint health disparities or outcomes to improve. For low-resource countries, this capability is crucial - it helps target interventions (for example, identifying which region has a spike in malaria cases or where maternal health outcomes are lagging). Paper records rarely yield such insights because the information remains locked in filing cabinets. Digital systems, by contrast, turn daily patient encounters into actionable data for improving care at both the patient and population level.
In short, electronic health records directly address the weaknesses of paper systems. They save time, reduce errors, improve collaboration, and generate data that can drive health improvements. These benefits are not theoretical - they are being observed on the ground in clinics that have made the switch, even in low-income and remote settings.
Real-World Examples from Africa, the Caribbean, South America, and Beyond
Digital health records are no longer a luxury limited to rich countries. Around the world, pioneering projects in low-resource settings have shown that "going digital" is both feasible and hugely beneficial. Here are a few notable examples:
- Sub-Saharan Africa: Across Africa, a number of countries are actively implementing EHR systems with promising results. Rwanda has been a frontrunner its digitization of diabetes clinics (mentioned above) led to measurable improvements in patient care. In Ghana, the Komfo Anokye Teaching Hospital adopted EHRs in its emergency department and reported better documentation accuracy and more timely care decisions. Many nations, from Kenya to Nigeria, have piloted open-source electronic record systems (like OpenMRS and others) in HIV clinics and general hospitals, improving the management of diseases such as HIV/AIDS and tuberculosis. While adoption in Africa is not yet widespread, momentum is building. Governments and NGOs, often with support from the WHO and international donors, are striving to enhance healthcare through EHR projects. The World Health Organization has stressed digital health as a priority for African health systems, and multiple studies across sub-Saharan Africa highlight significant benefits when EHRs are used, including better data management and patient care. Of course, challenges like infrastructure and cost remain (as we discuss later), but the success stories so far are encouraging other clinics to take the digital leap.
- Caribbean: Island nations have likewise begun transforming their health information systems. Jamaica recently launched a major Electronic Health Record initiative in 2023, backed by a US $50 million loan from the Inter-American Development Bank. This program aims for a "one patient, one record" system nationwide, and a UK-based tech company was contracted to deploy the platform. In Trinidad and Tobago, the government has integrated digital solutions across the health sector, including nationwide telemedicine services and linked databases, to improve efficiency and cut costs. Barbados has also been ahead of the curve - several public hospitals and clinics there use EMRs to manage patients, making it easy for any doctor to pull up accurate medical histories. Barbados even leverages telehealth so that people in rural areas can consult specialists without long travel. These examples show how Caribbean healthcare is closing the digital gap. The progress varies by country (some smaller islands are still largely on paper), but regional bodies like the Pan American Health Organization (PAHO) have been encouraging and supporting e-health reforms. The trend is clear: the Caribbean is moving towards modern, connected health record systems to serve their populations more effectively.
- South America: Latin America's healthcare systems are undergoing a digital transformation as well. By 2017, roughly 40% of hospitals in Latin America had an EMR system in place, up from 36% the year before , and the adoption has only accelerated since then. Chile is a standout, with some of the highest EHR penetration in the region (around 74% of healthcare facilities were using electronic records as of a few years ago). Uruguay implemented a national EHR platform in 2014 and achieved about 63% penetration across its healthcare facilities soon after a remarkable feat for a middle-income country. Brazil, which has a mix of high-tech urban hospitals and resource-poor rural clinics, made a multi-million dollar investment to unify all government health records into a single system. This included deploying supercomputers and setting national EHR adoption targets through 2020. The motivation in South America is both to improve care quality and to manage costs in public health systems. For instance, Argentina and Peru have also launched regional EHR projects to better track patient information in public clinics. The trajectory in Latin America demonstrates that even in resource-constrained environments, scaling up digital health records is possible with strong government commitment and strategic investments. The payoff has been improved coordination of care and better use of health data for decision-making.
- Egypt (North Africa): In Egypt, a country with a mix of urban centers and rural communities, digitization of health records has become a pillar of its health reform. The Egypt Healthcare Authority which oversees the new Universal Health Insurance system announced that it is now "fully digital," having created 4.5 million electronic health records for patients enrolled in the insurance program. They have also issued over 42 million electronic prescriptions through this system. This large-scale EHR rollout is part of Egypt's push to modernize its healthcare and ensure continuity of care for its citizens. By moving to a unified electronic platform, Egypt aims to eliminate the fragmentation of patient records and improve service delivery. The fact that millions of Egyptians already have digital records shows the scale that is achievable, even in a country classified as a lower-middle-income economy. It sets an example for neighboring regions that nationwide EHR implementation is within reach with the right strategy and leadership.
- Rural America: Even in high-income countries like the United States, rural and underserved areas often face challenges similar to clinics in developing countries including tight budgets, fewer IT staff, and patchy internet connectivity. Over the past decade, rural American clinics and small hospitals have been transitioning from paper to EHRs largely thanks to government incentive programs. By the mid-2010s, rural clinics had actually caught up with or even surpassed urban clinics in EHR adoption rates , propelled by federal "Meaningful Use" incentives. However, adoption is just the first step; many rural providers struggle with maintaining and optimally using their EHR systems. They often have limited financial resources and workforce shortages for IT. A 2024 report notes that rural healthcare organizations face ongoing hurdles like poor broadband access, interoperability issues, and cybersecurity concerns. Still, progress is undeniable: critical-access hospitals and community health centers across the U.S. now use EHRs to coordinate care. For example, in Alaska, remote village clinics use electronic records that can sync via satellite, and in Mississippi, a network of rural clinics shares a unified EHR to ensure migrant farmworkers' health data follows them. These efforts illustrate that whether in Mississippi or Malawi, digitizing health records is seen as a necessity for improving care in remote communities.
Each of these examples from Africa to the Americas reinforces the central message: digital health records are delivering real value in low-resource settings. Clinics that have made the switch report better efficiency and patient outcomes, which in turn drives more facilities to consider going digital. The movement is no longer isolated pilot projects; it's becoming a global standard of care.
Infrastructure and Training: Making the Transition Work
While the benefits of digital records are compelling, transitioning from paper to EHR is a significant undertaking. Health IT decision-makers must plan for the practical challenges of implementation, especially in low-resource environments. Two critical factors determine the success of this transition: infrastructure and training.
1. Infrastructure needs (power, hardware, connectivity).
A digital system is only as good as the infrastructure supporting it. Clinics need reliable electricity and computing devices (servers, PCs or tablets) to use EHRs consistently. In many rural or remote areas, power outages or voltage fluctuations are common which means investing in generators or solar backup systems to keep the computers running. Equally important is internet connectivity: if an EHR is cloud-based or needs to share data with other sites, it requires a stable network. Unfortunately, the "digital divide" is real. In the United States, for example, only about 73.6% of rural Americans had access to broadband internet at baseline speeds in 2019, compared to 96% of the overall population. The gap can be even wider in parts of sub-Saharan Africa or mountainous regions of South America. This lack of broadband infrastructure can hinder the use of advanced EHR features like health information exchange or telehealth. To address this, some low-resource settings use offline-capable EHR solutions - systems that can run on a local network and sync data whenever a connection becomes available. Others leverage mobile networks, which have leapfrogged landlines in many developing regions, to transmit data. It's also possible to start with a standalone digital system (within one hospital, for instance) if wider connectivity is not yet in place, and expand integration gradually. The key is to ensure that lack of perfect infrastructure doesn't halt the march toward digitization. With creative planning (like using local servers, caching data, or installing satellite internet for remote clinics), even resource-limited areas can support robust digital health records.
2. Training and change management.
Transitioning to an EHR is as much about people as technology. Clinic staff - doctors, nurses, clerks - need to be comfortable with the new system. In low-resource settings, computer proficiency may vary widely. Ample training and support must be provided so that users gain confidence in using the software for registration, data entry, and retrieval of information. One study found that nearly two out of three rural primary care practices reported their staff needed more training to effectively use EHRs, but access to training resources in underserved areas was limited. This highlights the necessity of budgeting time and funds for user education. Effective strategies include initial and ongoing training sessions and a "train the trainer" model. For example, implementing teams often identify local "EHR champions" staff members who are enthusiastic and tech-savvy and give them advanced training. These champions then serve as on-site support for their colleagues, helping to troubleshoot issues and encourage proper use of the system. This approach was recommended in a study on EHR adoption in Africa: start training with the most interested users, develop them into super-users, and let them mentor others. It not only spreads knowledge but also builds buy-in among staff. Another consideration is workflow redesign. Simply digitizing a bad manual process won't yield better results; staff might need guidance on new workflows (for instance, how to enter data in real-time during a patient exam, which is a change from scribbling notes to file later). Change can be daunting some older or less tech-comfortable workers may resist. It's important to communicate the benefits clearly and to provide continuous support. Many successful projects have phased rollouts (starting with one department or module) to let people adjust gradually. In sum, human capacity building is paramount: without well-trained, motivated users, even the best EHR system will falter.
3. Technical support and sustainability.
Along with training, clinics need a plan for technical support and maintenance. Computers freeze, software has bugs, and users will have questions. Urban hospitals might have an IT department, but a rural clinic likely does not. This is where partnerships and creative solutions come in. Some low-resource regions set up regional support centers or use a "hub and spoke" model where a central hospital's IT team remotely supports peripheral clinics. Others rely on the EHR vendors or open-source communities for help. During the U.S. EHR rollout, Regional Extension Centers were established to assist rural providers in implementing EHRs a model that could be replicated by NGOs or governments in other countries. It's also wise to budget for ongoing costs: system updates, cloud service fees (if applicable), device replacements, etc. Many hospitals and physicians in sub-Saharan Africa have been concerned about the costs of hardware, software, installation, and connectivity, as well as ongoing support fees. Decision-makers should explore cost-effective options such as open-source software (which has no licensing fees) and cloud-hosted solutions (which reduce the need for on-site servers). Moreover, demonstrating the long-term savings of EHRs for example, reductions in paper storage costs, transcription costs, or avoidance of costly medical errors can help justify the investment. In practice, numerous donors and government grants are available to support health IT upgrades in low-income settings, as seen with the IDB loan for Jamaica's EHR project. Tapping into these resources can alleviate the financial burden.
Ultimately, the transition from paper to digital is a journey, not an overnight switch. It requires strong leadership, careful planning, and stakeholder buy-in. However, with solid infrastructure planning and a focus on training and support, even resource-limited clinics can successfully make the leap. The experience from various countries has shown that challenges like unreliable internet or limited IT staff can be overcome with the right strategies and the reward is a health system that is more efficient, connected, and resilient.
Affordable EHR Solutions Tailored for Low-Resource Clinics
One encouraging aspect for clinics considering the move to digital is the availability of affordable and adaptable EHR solutions. Not all systems are expensive proprietary products; some trusted platforms are low-cost or even free, and have been designed with resource-limited settings in mind. Open-source software has been a game-changer in this arena. OpenEMR - for example - is the world's most popular open-source electronic health record and medical practice management software. As an open-source platform, OpenEMR can be downloaded for free and customized to local needs without paying license fees. It has a community of volunteers and developers who continuously improve it, and it's used by clinics worldwide, including many in developing countries. For health ministries or NGOs, open-source EHRs offer a budget-friendly option that can be locally hosted and even run on basic hardware. They also provide flexibility: features can be added or modified, which is useful when adapting to unique workflows or languages.
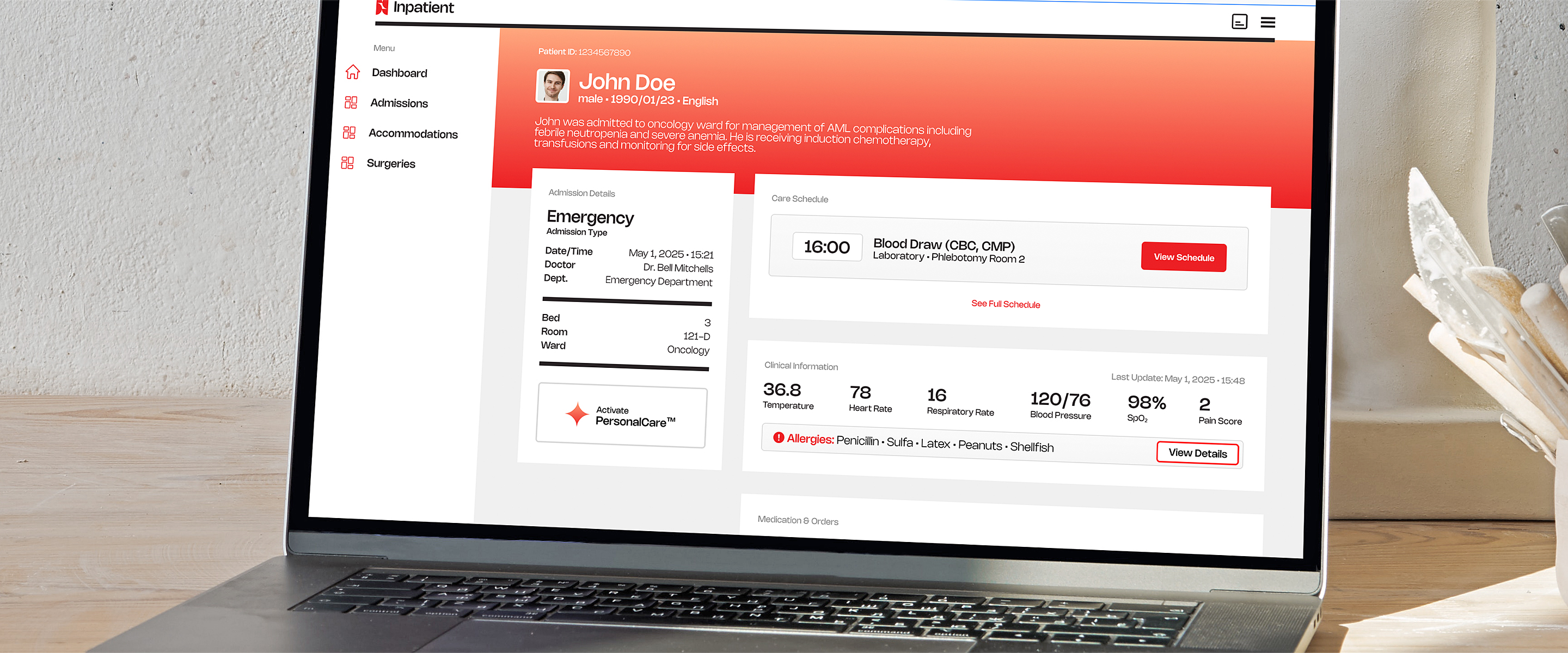
Building on open-source foundations, some organizations have created tailored solutions for low-resource settings. A great example is MedSov, an advanced EHR and clinic management system that is powered by OpenEMR and adapted specifically for low-income markets in Africa and the Caribbean. MedSov was developed by Omega Systems Group (also known as Omega Global Health Technologies), an IT firm that focuses on open-source healthcare solutions. Omega Systems Group leveraged OpenEMR's robust base and added customizations to meet the needs on the ground things like offline capabilities, simplified interfaces for clinics with limited staff, and modules relevant to local health priorities. By doing so, they created a solution that offers the reliability of a proven EHR core with the usability required in, say, a remote Ugandan health center or a small clinic in Haiti. The existence of MedSov and similar products demonstrates that companies are responding to the call for context-appropriate digital health tools. They prove that one doesn't need a Silicon Valley budget to implement a quality EHR; with the right expertise, even a modest clinic can have a system that rival those in big hospitals.
Additionally, several international initiatives and products cater to this space. For instance, OpenMRS (Open Medical Record System) not mentioned earlier is another open-source EHR platform that has been widely implemented by NGOs in Africa and South Asia. There are also cloud-based services aimed at NGOs and small clinics, which operate on a subscription model at low cost (sometimes even free for the smallest facilities). The advantage of cloud-based solutions is that they reduce the need for on-site IT infrastructure (just a device with internet access is needed), although they do require that connectivity.
When choosing a solution, decision-makers should consider factors such as: cost, language support, ease of use, available support/training, and alignment with national reporting requirements. For example, an EHR that can easily generate the reports required by the Ministry of Health (for disease surveillance or inventory management) will save a lot of time. It's also prudent to pilot the system in one or two sites first, to gather feedback from staff and ensure it meets the needs, before scaling up broadly. The good news is that with options like OpenEMR , MedSov by Omega , and other open-source or low-cost platforms, clinics in low-resource settings have a menu of viable choices. These systems are trusted in the sense that they are used by many and backed by active communities or companies. By opting for such solutions, a health facility can avoid being locked into expensive vendor contracts and instead invest more in training and sustaining the system. In summary, the technological tools for digital records exist and are within reach - it's now a matter of will and execution to put them into action.
Conclusion: From Paper to Digital - An Urgent and Valuable Transition
The writing is on the wall (or rather, in the cloud): the era of paper health records is drawing to a close, even for clinics in low-resource settings. The inefficiencies and risks associated with paper-based systems - lost files, wasted time, data silos, and vulnerability to disasters are simply untenable in a world striving for better health outcomes and greater accountability. Digital health records offer a clear pathway to address these issues, bringing immediate improvements in efficiency, safety, and quality of care. They empower healthcare workers with information at their fingertips, enable health administrators to make data-driven decisions, and help patients receive more coordinated, continuous care. As we have seen, countries and clinics that have embraced EHRs are already reaping these rewards, from a rural hospital in Rwanda to a polyclinic in Trinidad to community practices in Appalachia.
For health IT decision-makers - whether you are a Ministry of Health official, a hospital director, or an NGO program manager - the case for transitioning to digital records is compelling and urgent. Yes, the journey requires investment in infrastructure and training, and there will be challenges to navigate. But the experiences of peers around the world show that these challenges can be overcome with planning, partnerships, and perseverance. Moreover, the cost of inaction is growing: each day on paper is a day of missed opportunities - missed diagnoses due to inaccessible records, wasted funds on repeated tests, and missed chances to analyze health trends in your community. In contrast, adopting a robust EHR system opens doors to innovations like telehealth, mobile health integration, and real-time disease surveillance, all of which are crucial for resilient healthcare systems in the 21st century.
It's often said that health data is the "lifeblood" of a system and in low-resource settings, making that lifeblood flow effectively can literally save lives. By moving from paper to digital health records, clinics are not just keeping up with technology; they are building the foundation for smarter healthcare. The transition signals to healthcare workers and patients alike that their information will not be lost or forgotten, but instead will be used to provide the best possible care wherever and whenever it's needed. In conclusion, the shift to digital health records in low-resource settings is more than a technical upgrade - it's a leap toward health equity and excellence. The tools and knowledge to make this leap are available, and the success stories are accumulating. The question is no longer if clinics should move away from paper, but how quickly can we make it happen. Those who act with urgency and vision will position their health systems to save more lives, operate more efficiently, and meet the health challenges of the future with confidence. The time to turn the page (or rather, to click "save" on the EHR) is now.